When it comes to protecting your smile, early treatment makes all the difference. From routine exams and cleanings to advanced treatments like Invisalign, dental implants, and professional whitening, our goal at Chester Springs Dental is to help you maintain a healthy, confident smile for life. One of the most common and effective ways we preserve natural teeth is through dental fillings — a simple solution that stops decay, restores strength, and prevents bigger dental problems down the road.
What Are Dental Fillings?
Dental fillings are a restorative treatment used to repair cavities, minor cracks, or damaged areas of a tooth. After removing decay, your dentist fills the space with a durable material that restores function and protects the tooth from further damage. Fillings not only strengthen teeth but also help preserve your natural smile and chewing ability.
As Dr. Richard Gross explains:
“A dental filling is often the most conservative way to save a tooth. When we treat decay early, we can protect the natural tooth structure and help patients avoid more extensive procedures in the future.”
Types of Dental Fillings
There are two main categories of fillings, and the right option depends on your needs, budget, and oral health goals:
- Direct fillings (placed in one visit):
- Composite resin (tooth-colored)
- Amalgam (silver)
- Glass ionomer
- Indirect fillings (custom-made in a lab):
- Porcelain inlays or onlays
- Gold restorations
Many modern fillings are designed to blend seamlessly with your natural teeth and can last 10–20 years with proper care.
What to Expect During the Procedure
Getting a filling is typically quick and comfortable. The area is numbed, decay is removed, and the filling material is placed, shaped, and polished. Most patients return to normal activities the same day. Mild sensitivity afterward is normal and temporary.
If dental visits make you anxious, our team is happy to discuss comfort and sedation options — your peace of mind matters to us.
Why Prompt Care Matters
Cavities don’t heal on their own. Left untreated, they can lead to pain, infection, or the need for more complex treatments like root canals or crowns. Dental fillings stop decay in its tracks and help you maintain long-term oral health.
To stay connected with smile tips, office updates, and patient education, follow us on Instagram:
👉 https://www.instagram.com/chesterspringsdental
Personalized Care for Our Community
We proudly serve patients in Exton, Chester Springs, Lionville, Downingtown, and surrounding communities, offering personalized treatment plans and flexible options — even if you don’t have dental insurance. Our Membership Savings Club helps make quality dental care more affordable and accessible.
As Dr. Gross often reminds patients:
“Comfort, trust, and education are just as important as treatment. When patients understand their options, they feel confident taking the next step toward better oral health.”

Take the Next Step
If you suspect a cavity, have tooth sensitivity, or it’s simply time for a checkup, we’re here to help. Prompt care today can save you time, discomfort, and expense tomorrow.
📞 Schedule your appointment with Dr. Richard Gross today: 610-524-9530
📧 Email: office@chesterspringsdental.com
🌐 Visit us online: https://chesterspringsdental.com/
Protect your smile this February — because strong, healthy teeth are always worth it.










 You’ve got the tips to navigate the holidays safely. Now, ensure your smile is truly ready to shine for every festive gathering and photo opportunity! We’ll inspect your cosmetic and restorative work, leaving your smile vibrant and perfectly maintained. Schedule your appointment with Dr. Richard Gross’s dental services today at 610-524-9530 or join our Instagram community
You’ve got the tips to navigate the holidays safely. Now, ensure your smile is truly ready to shine for every festive gathering and photo opportunity! We’ll inspect your cosmetic and restorative work, leaving your smile vibrant and perfectly maintained. Schedule your appointment with Dr. Richard Gross’s dental services today at 610-524-9530 or join our Instagram community


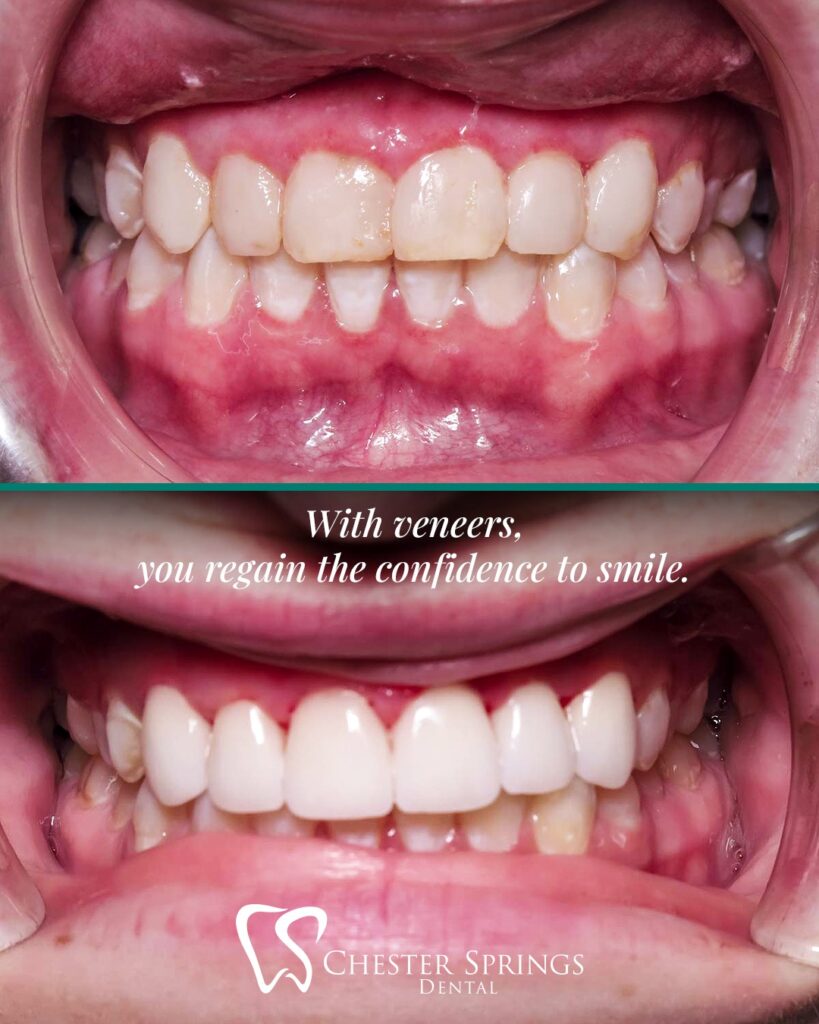 Restore Your Smile with Confidence
Restore Your Smile with Confidence









 When is an oral cancer screening recommended?
When is an oral cancer screening recommended?