Tooth extraction may be necessary in various dental situations. This procedure involves the removal of a tooth from its socket in the jawbone. Some common reasons for tooth extraction include severe tooth decay or infection that cannot be treated with other methods. Learn here the common indications for tooth extraction and provide valuable information to help you understand when this procedure may be necessary.
Considering a tooth extraction can feel overwhelming—but at Chester Springs Dental, we’re here to answer all your questions and ensure you feel completely comfortable. Dr. Gross and Dr. Hudson put patients first because, to us, “Attached to every tooth is a person.”
Reach out to meet our caring team and experience our patient-focused approach. You’ll feel welcomed and reassured from the moment you connect with us. 610.524.9530
What is a tooth extraction?
A tooth extraction is a dental procedure during which your tooth is completely removed from its socket. Sometimes, people refer to this as “pulling” a tooth.
When is tooth extraction recommended?
Healthcare providers prefer to save natural teeth whenever possible. But sometimes, other restorative methods — such as dental fillings or dental crowns — aren’t enough. If your tooth has been badly damaged past the point of repair, then removal may be necessary. Your dentist may recommend tooth extraction if you have:
- Severe tooth decay (cavities).
- A fractured tooth.
- An impacted tooth.
- Crowded teeth.
- Severe gum disease.
- Tooth luxation or other dental injuries.
Who performs tooth extraction?
Dentists and some dental specialists — such as oral surgeons and periodontists — can perform tooth extractions. While general dentists perform plenty of extractions, more complex cases are usually referred out to oral surgeons or periodontists.
Procedure Details
What happens before a tooth extraction?
Your dentist will assess your affected tooth and surrounding gums. Your dentist will also take dental X-rays to check bone levels and determine the extent of damage. Be sure to tell your dentist about any medications, vitamins or supplements you’re taking. Once all information is gathered, treatment and sedation options will be discussed with you in detail.
Sedation options in dentistry
Many healthcare providers offer sedation during tooth extractions and other dental procedures. Sedation is an excellent option for people who have dental anxiety — or for those who simply want to be more comfortable during their appointment. Sedation medications used in dentistry include:
- Nitrous oxide. Known as “laughing gas,” nitrous oxide is a gas that you inhale through a mask or nosepiece. It’s a good option for people who need light level sedation. People who choose nitrous oxide can drive themselves to and from their appointments.
- Oral conscious sedation. This type of sedation is given by mouth, usually in pill form, about an hour before your dental appointment. Common medications used for this purpose include diazepam, midazolam, triazolam and lorazepam. Oral conscious sedation can be used on its own or in combination with nitrous oxide or intravenous sedation. Dosages are adjusted according to your specific needs. People who choose oral conscious sedation will need a friend or family member to drive them to and from their appointment.
- Intravenous (IV) sedation. This is recommended for people with significant dental anxiety or for those undergoing lengthy procedures. Sedative and pain medications — such as midazolam and meperidine — are delivered directly to your bloodstream using an IV line. IV sedation is the highest level of sedation that can be obtained in a dental office setting. People who choose IV sedation will need to make arrangements for a driver the day of their procedure.
In some instances, your dental provider may recommend general anesthesia in a hospital setting. This option is usually reserved for complex cases, such as facial reconstruction or corrective jaw surgery.
What happens during a tooth extraction?
First, local anesthesia is given to numb your affected tooth and surrounding gum tissue. Using specialized dental instruments, your dentist will gently loosen your tooth and carefully lift it from its socket. Sometimes, your dentist might need to make incisions in your gums to access your tooth — especially if your tooth is badly decayed or has broken off at the gum line. Once your tooth is removed, the socket is cleaned and disinfected. In some cases, your dentist may also place a dental bone graft, which helps prevent bone loss in your jaw. Finally, stitches may be placed to help promote healing.
What happens after a tooth extraction?
When the procedure is complete, your dentist will place a piece of gauze over the extraction site and ask you to close down with firm, steady pressure. This helps slow bleeding so a blood clot can form. (Clotting is a normal aspect of recovery. It promotes healing and reduces the risk of dry sockets.) You’ll take the gauze out once the bleeding has slowed enough. You may continue to have light bleeding throughout the first 24 hours.
Risks / Benefits
What are the advantages of pulling a tooth?
Tooth extraction offers a number of benefits. Most importantly, it reduces harmful bacteria that can damage your teeth and gums. Left untreated, a decayed or damaged tooth can wreak havoc on your smile, causing a domino effect of problems. Removing your affected tooth gives you the best chance for optimal oral health. Additionally, a tooth extraction can help ease dental pain almost immediately — especially if your tooth was severely broken or infected.
What are the risks or complications of tooth extraction?
Like any surgical procedure, tooth extraction carries a small risk of complications. These may include:
- Post-surgical infection.
- Dry socket.
- Nerve injury.
- Perforation of maxillary sinus.
- Delayed healing.
What are the side effects of removing a tooth?
Normal side effects following tooth extraction include bleeding, swelling and discomfort. Your dentist will provide instructions on how to successfully manage your healing.
Recovery and Outlook
How long does it take to recover from a tooth extraction?
It depends on the complexity of your case. However, most people feel back to normal in just a few days. While you’ll be able to return to routine activities within 48 to 72 hours, it usually takes the jawbone several weeks to heal completely. Therefore, if you’re planning on replacing the tooth with a dental implant, you’ll probably need to wait a few months to allow for full recovery.
Tooth extraction aftercare
After your extraction, your dentist will give you a detailed list of post-surgical instructions. Here are some general guidelines for a speedy recovery:
- Keep the extraction site clean. Gently rinse the area with an antimicrobial mouthwash two to three times a day. Avoid brushing directly over your extraction site until your dentist tells you it’s safe to do so. Brush and floss all other areas normally.
- Take all medications as directed. Your dentist may prescribe antibiotics and pain relievers. It’s important to take all of these medications exactly as directed. You can also take over-the-counter pain relievers, such as acetaminophen and ibuprofen.
- Avoid strenuous activity for at least two days. An elevated heart rate can cause increased post-operative bleeding and discomfort. Skip the gym for the first 48 to 72 hours. Ask your dentist when it’s safe to resume normal routines.
What can I eat after a tooth extraction?
Avoid hard and crunchy foods for the first few days. Stock your fridge and pantry with soft foods like rice, pasta, eggs, yogurt and applesauce. You’ll also want to avoid drinking through straws, as this can dislodge blood clots and cause dry sockets.
When can I go back to work or school?
Most people are able to return to work or school within a day or two. If you have a job that requires a lot of lifting or physical labor, you may need to take a few more days off work.
When To Call the Doctor
When should I see my healthcare provider?
Any time you develop a toothache or dental pain, it’s important to schedule a visit with your dentist. They can help determine the cause and design a personalized treatment plan.
If you’ve already had a tooth extraction, call your dentist if you develop a fever of 100.4 degrees Fahrenheit (38 degrees Celsius) or higher, drainage (pus) around the extraction site or severe pain that doesn’t improve with medication.
A note from Cleveland Clinic
It’s never fun hearing that you need to have a tooth pulled. But sometimes, a tooth extraction is the best way to eliminate infection and get you back on track to a healthy smile and life. If your dentist recommends an extraction, be sure to discuss replacement options with them, too. Dental restorations like dental implants, dental bridges or partial dentures can restore appearance, function and overall oral health.
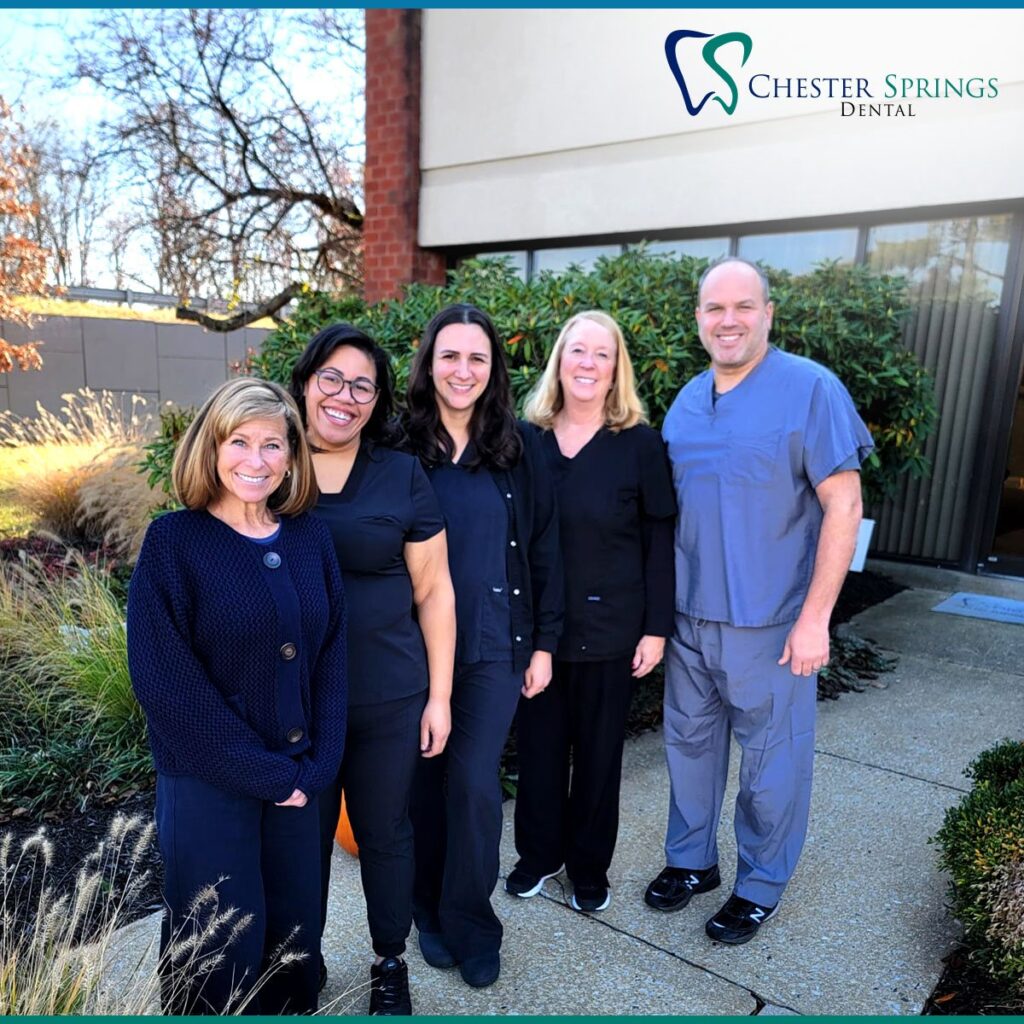
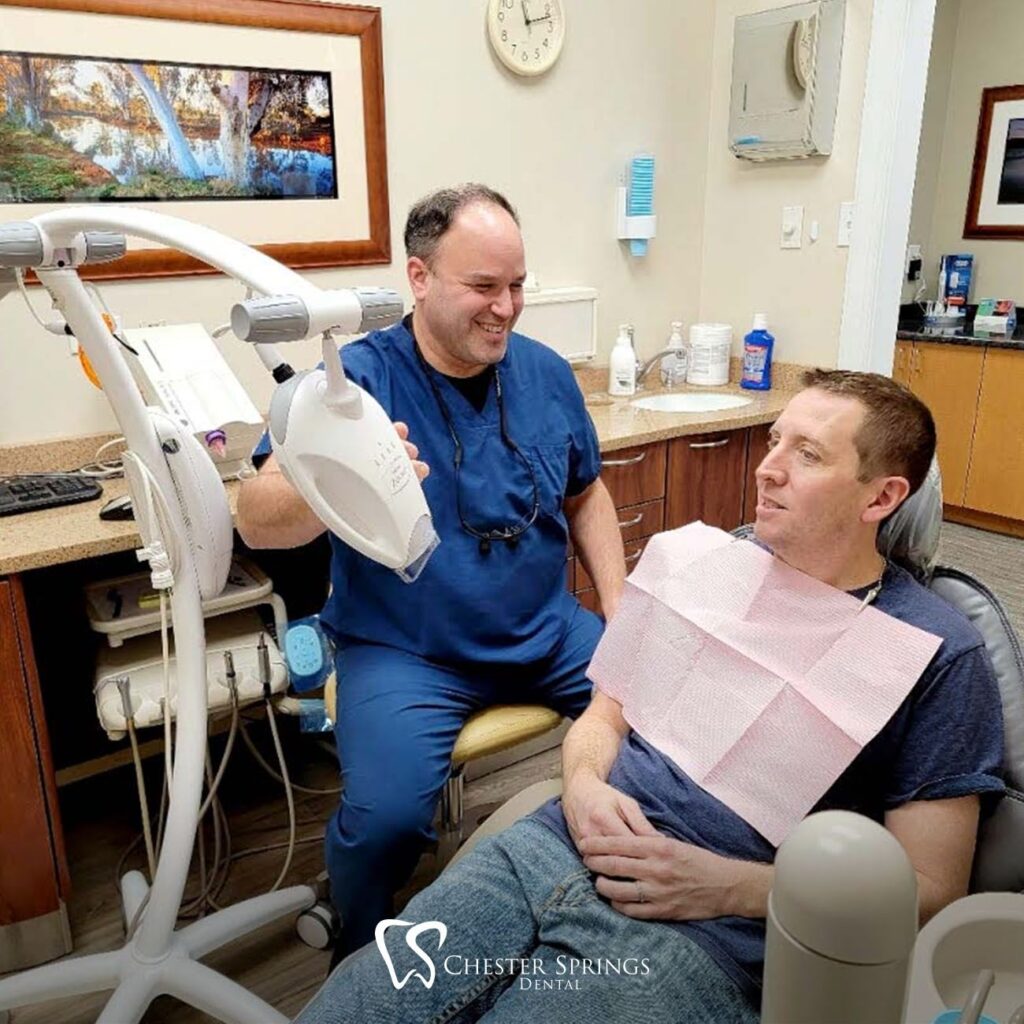
Meet Dr. Gross!
Concerned about a tooth extraction? Our advanced techniques and experienced team minimize discomfort and ensure a smooth and successful procedure. We invite you to reach out and meet our compassionate team. From your first contact, you’ll feel welcomed and supported every step of the way. Schedule your appointment with Dr. Richard Gross dental services today at 610-524-9530 or office@chesterspringsdental.com Join our Instagram community here!
Reference: [https://my.clevelandclinic.org/health/treatments/22120-tooth-extraction]